Reverse Total Shoulder Replacement
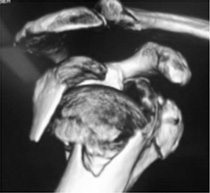
Shoulders that are worn out can be replaced just like hips or knees. The reverse shoulder replacement was developed for people with painful shoulders who had rotator cuff tears and shoulder arthritis that failed to respond to non-operative measures.
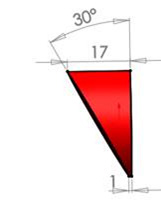
Traditional “anatomic” shoulder replacement was unsuccessful in patients with large rotator cuff tears due to early implant loosening. By reversing the ball and socket a more stable joint was created that could restore pain relief and shoulder function.
 Anatomical replacement
Anatomical replacement Reverse replacement
Reverse replacement
Over time the reverse replacement has proven to be a durable implant and the use has expanded to include more conditions: Complex shoulder fractures and fracture complications
Osteoarthritis with advanced bone wear
Osteoarthritis with poor rotator cuff tendon or muscle quality
Irreparable rotator cuff tears
The procedure is performed to restore quality of life. Just like hip replacement surgery the reverse total shoulder replacement provides excellent pain relief as the worn joint surfaces are separated by the stable metal on plastic articulation. The mechanics of the reverse joint helps residual rotator cuff and deltoid muscle restore above shoulder function.
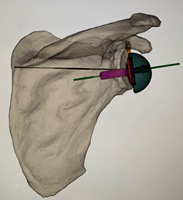
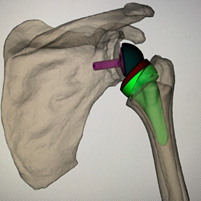
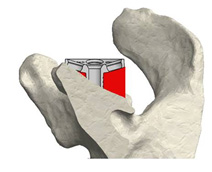
Prior to any appointment, a shoulder x-ray and ultrasound will suffice for investigations. If further investigations are required these can be organised at the appointment. If you elect to proceed with a reverse shoulder replacement, I will obtain a specific CT sequence of the shoulder and elbow. Using this CT scan a computer program can be used to determine implant position, size, movement and produce 3D printed guides.
3D planning
The 3D printed guides clip onto the humeral head and socket, at the time of surgery, to help accurately replicate the computer based surgical plan.
3D printed jigs
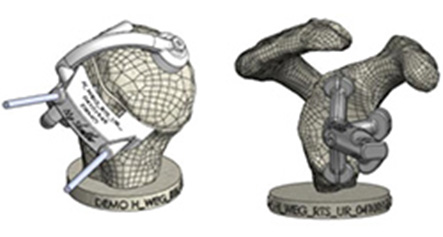
If there is significant bone wear from the arthritis, the defects can be filled with bone from the resected humeral head. The diameter, thickness and orientation of the bone graft can also be computer planned.
The surgery is performed with general anaesthesia and arm block. The surgery takes 90 mins - 3 hrs depending on complexity. Most patients are discharged home after 2 nights stay in hospital. Patients note after the surgery there chronic deep-seated arthritic pain has gone. There is pain from the surgical procedure but this settles quickly. Initial post-operative pain killers are usually opiate based and can cause constipation. A high fibre diet and additives (Coloxyl, Movicol) are encouraged. Simple pain killers are generally required for discharge. Rehabilitation or respite hospital transfer is rarely required. The wound is covered with a waterproof dressing that allows showering the day after surgery. The dressing should remain intact until the 2 weeks review. Bruising can be seen extending down the arm and this is normal. A sling is required for a variable time after surgery (maximum 6 weeks). Driving can be gradually restored after sling removal and stopping pain medication. Patients are instructed in a stretching program that can be self-directed. Formal physiotherapy is optional. Aggressive strengthening is discouraged because of the risk of a scapula stress fracture that can irreversibly damage the operation outcome.
Risks of the surgery, specific to the procedure are low but include infection, stiffness, nerve and vascular injury, fracture and dislocation. In an elderly population, the general risks of stroke and heart attack are higher. A pre-operative review by any treating specialist (eg. Cardiologists) is recommended. Patients may outlive the lifespan of the artificial joint. Approximately 80% of implants were retained at 15 years after insertion. The longevity should improve with better plastics and design.
PREPARATION FOR SURGERY
Things to consider
- If the surgery is on your dominant arm. Practicing tasks with your other arm in the weeks leading up to surgery will assist with independence in activities of daily living.
- If there are concerns regarding suitability for surgery, post-operative aftercare or care of a partner, a pre-operative review with a Geriatrician specialising in orthopaedic care and community support can be arranged.
- Meals can be prepared prior to surgery to minimise cooking loads in post-operative period.
- Sleeping can be difficult in a sling after surgery. Some patients find it easier sleeping in a recliner, that can be hired. Extra pillows can be used to pack around the arm.
- Risk for infection can be further reduced prior to surgery by showering and washing the shoulder with Benzac AC 5 % wash for 3 days prior to the surgery.

REHABILITATION
After the surgery you will be placed in a sling.
From the first day after surgery you will commence elbow and shoulder range of motion exercises.
Stage 1
Repeat each exercise 10 times. Do 3 sessions a day.
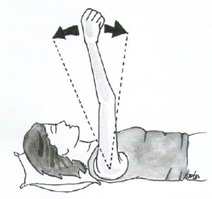
Passive Shoulder Elevation 1:With the help of someone, relax your arm completely while they slowly lift your arm as comfortable and lower it again. You should be aiming to get to 90 degrees to your body unless told otherwise. |
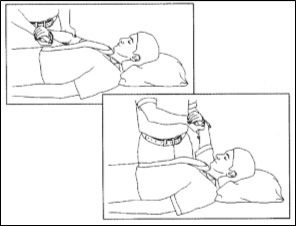 |
Passive Shoulder Elevation 2:Relax with your arm across your chest supported by your other arm. Slowly lift your arm as comfortable and lower it again. You should be aiming to get to 90 degrees to your body unless told otherwise |
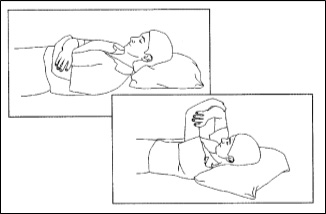 |
Passive Shoulder Elevation 3:In either sitting or standing, support your operated are with your other arm. Lean forward to allow gravity to assist you to lift your arm as comfortable and lower it again. You should be aiming to get to 90 degrees to your body unless told otherwise |
 |
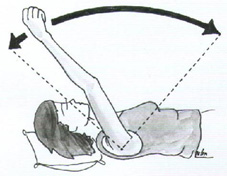
Stage 1
Shoulder External Rotation:Relax your arm completely with your hand resting on your stomach. Keep your elbow by your side and with the help of your other arm rotate your hand from your stomach so that it is pointing out from your body. Relax as you return your arm to rest on your stomach. |
 |
Elbow bending/straightening:With your arm resting on your stomach, slowly straighten your elbow as far as you can, then bend your elbow again. Keep the palm of your hand facing your body. You may be instructed to do this exercise with the assistance of the other hand depending on what type of surgery you have had. |
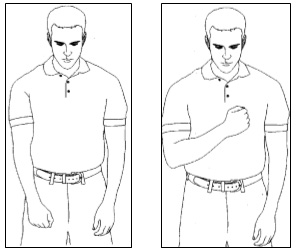 |
Wrist and Finger Movements:
|
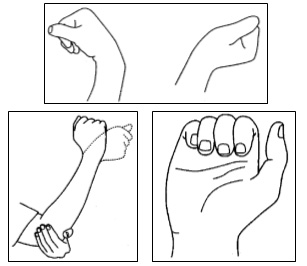 |
After the sling is removed a gentle stretching program can commence. No weights or resistance bands are required
LONG TERM CONSIDERATIONS
- Lifting limit: one off lifts should be less than 10kg. Repetitive lifts should be limited to less than 2 kg.
- Sports with low impact (eg. swimming and golf) can be gradually resumed as strength and endurance improves. Most return to these activities 4-6 months after surgery.