Shoulder Tendon Pain
What is a Shoulder Tendon?
A tendon is the white fibrous tissue that connects muscle to bone and is capable of withstanding significant tension. Tendons are made of collagen and together with the muscles they work to move bones.
Common tendon problems include:
- Tendinopathy
- Tears
What is Tendinopathy?
Tendinopathy is the replacement of normal tendon collagen with scar from overuse or aging. The scar may not cope with the muscle tension placed on the degenerate tendon, causing the tendon to fail or tear through the scar.
Rotator cuff tendinopathy is more common in people make the same repetitive overhead motions in their jobs, sport or daily activities.
The overloaded tendon progresses through four phases of tendon injury.
- Reactive Tendinopathy
- Tendon Dysrepair
- Degenerative Tendinopathy
- Tendon Tear or Rupture
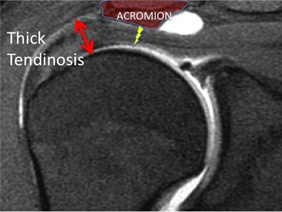
Normal healthy black tendon Thickened grey tendinosis
Tendinopathy Symptoms
Tendinopathy causes the following symptoms:
- pain
- stiffness
- loss of strength in the affected area.
- worsening pain with tendon use
- shoulder tenderness
- audible crunchy sound or feeling with movement.
You may have more pain and stiffness at night or when you get up in the morning.
Tendinopathy can affect other tendons throughout the body, including :
- Quadriceps tendon
- Archilles Tendon
- Biceps tendon
Diagnosis of Tendinopathy
The diagnosis of tendinopathy requires:
Consultation - During this consultation Dr Harper will:
- take a medical history, with emphasis on pain , loss of function and treatments.
- a physical examination, documenting range of motion, strength and shoulder impingement
Imaging tests - In order to clearly understand the state of the rotator cuff tendons or bone spur formation imaging scans are required:
- X-rays - do not show tendons but may show changes in the shoulder blade shape that narrows the tunnel over the rotator cuff tendons. X-rays also show arthritis of the ball and socket or collar bone / shoulder blade (AC) joint that can also cause shoulder pain.

Acromial spur with overhang and narrowing of the tendon tunnel
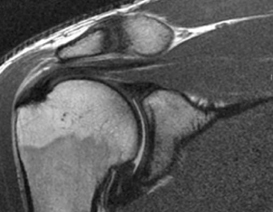
- Ultrasound - can visualise the rotator cuff tendons, compare both shoulders and examine the tendons with arm motion.
- MRI - can create detailed images of both hard and soft tissues. An MRI can produce cross-sectional images rotator cuff tendons, if the diagnosis is unclear or surgery is being considered.
While not all of these approaches or tests are required to confirm the diagnosis, this diagnostic process will also allow Dr Harper to review any possible risks or existing conditions that could interfere with the surgery or its outcome.
Treatment for Tendinopathy
Non surgical treatments can include:
- Resting the painful area
- Avoiding activities that makes the pain worse
- Pain management: including analgesics, anti-inflammatory medications and thermal ( hot or cold) packs
- Stretching to prevent stiffness
- Gentle strengthening program
Surgery for prolonged Tendinopathy
If non-operatives measures have been exhausted and the pain associated with tendinopathy is grossly affecting quality of life, surgical options can be considered. The principal surgical procedure for rotator cuff tendinopathy is removing an abnormal bone shape or spur from the tunnel over the tendons, created by the shoulder blade. This surgical procedure is known as an acromioplasty. If the tendinopathy has progressed to tendon tears then tendon repair surgery may also be required.
Untreated Tendinopathy
Tendinopathy is not life threatening but can severely impact a patient’s quality of life and function.
It can affect anyone: elite athletes and the active individual, manual labourers and office workers. Chronic tendon pain can interfere with employment, sleep and pastimes.
Surgery Risks with Tendinopathy
Prior to making any decision to have surgery, it is important that the patient discusses any concerns with Dr Harper and understands the potential risks.
While complications due to surgery are uncommon they can occur, the following are some:
- infection
- joint stiffness
- local nerve or blood vessel damage
- Incomplete pain relief
- reflex sympathetic dystrophy
Rarely do these complications prevail over the long term. Other general medical and surgical risks can include:
- risk of chest infection
- bleeding and clots in the arm, leg (DVT) or lung post-operatively
- allergies and anaesthetic complications can occur
If there are any postoperative concerns or pain please do not hesitate in contacting the doctors rooms or hospital.
Preparing for Tendinopathy Surgery
If surgery is required, preparation is necessary to achieve the best results and recovery.
Preparing mentally and physically for surgery is an important step toward a successful result.
- Dr Harper will outline the treatment plan and
- patients will need to understand the process and their participation.
Performing a tailored exercise program before surgery (ie. pre-hab) with a physiotherapist may assist with surgical recovery.
Dr Harper will also need to:
- discuss any medications being taken, to see which ones should be stopped before surgery
- do not eat or drink anything, including water, for 6 hours before surgery
- stop taking aspirin, warfarin, anti-inflammatory medications or drugs that increase the risk of bleeding one week before surgery to minimise bleeding
- stop or cut down smoking to reduce your surgery risks and improve your recovery
Report any infections (dental, skin, chest, urinary) to Dr Harper prior to surgery as the procedure cannot be performed until all infections have cleared up.
After Your Operation:
Recovery
Some patients need one night in hospital, although it is possible to leave hospital the day of surgery. The incision wounds take 10 days to heal.
Most patients improve dramatically in the first 6 weeks. Occasionally, there are periods where the shoulder may become sore and then settle again. This is part of the normal healing process.
It takes three to four months for the patient's shoulder to recover from surgery.
Continued improvements may be gained up to 1 year post-surgery.
Complications
Dr Harper should be contacted if any postoperative problems occur. These include redness, increasing pain or fevers. If unavailable, seek advice from the hospital or your general practitioner.
Pain Management after Surgery
A patient’s experience of pain will vary depending on the procedure performed and the amount of pre-existing damage. Local anaesthetic is injected before and after the procedure to minimise any pain you may feel. After your operation you will have pain medications. These will include paracetamol, anti-inflammatory medication and opiate medications if there are no allergies. These medications can be taken in combination as per directions. Anti-inflammatory medications should be taken with food to avoid gastric irritation. Opiate medications can cause constipation, that can be reduced by increasing hydration and dietary fibre. These medications should be reduced as pain subsides.
Mobility
Lifting- After surgery, the patient’s arm may be placed in a sling for a short period of time. As soon as comfort allows you can remove the sling to begin exercise and use of the arm.
Walking - is allowed immediately.
Driving - do not drive for 48 hours after an anaesthetic. After 48 hours, ability to drive will depend on the area you had your operation, left or right, and the type of vehicle driven, manual or automatic. Otherwise, it is reasonable to drive when the patient is confident and the sling is no longer required.
Return to Work After Surgery
Return to work will vary depending on the procedure performed and type of work the patient is engaged in. Most people can return to office work within 2 weeks. Labour intensive work may require the patient to take 3 months before returning to full duties.
During this period patients are not fit to perform work duties that involve:
- heavy lifting,
- Overhead activity
- repetitive upper arm activity
Return to Sport
In the first 2-4 weeks after surgery emphasis is placed on wound healing and restoring a normal range of movement. Low impact activities, such as cycling and swimming, can be commenced from week 4. If your procedure involves bone removal, high impact activities, such as throwing or lifting are best avoided for 6 weeks post-surgery.
Sport specific re-training can commence from week 6, with the aim to return to sports 3-4 months post-surgery.